Research
Recurrent non-invasive breast tumours may not always be related to the primary tumour
3 min read 12 April 2022
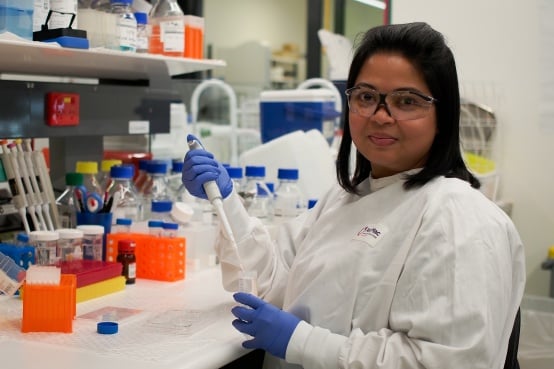
Patients with recurrent tumours genetically distinct from the primary tumour may require different treatment. More than 10 per cent of cases of recurrent ductal carcinoma in situ (DCIS) of the breast were new tumours occurring independently of the primary lesion and had distinct genetic alterations, according to Peter Mac research presented at the AACR Annual Meeting 2022 earlier this week. "DCIS is a precancerous lesion that recurs in approximately 25 per cent of patients, and half of these recurrences are invasive cancer with potential life-threatening consequences," says postdoctoral researcher Dr Tanjina Kader who presented the work. According to Dr Kader, it had been assumed that all recurrent tumours occurring in the same breast were directly related to the original tumour but never proven. "Knowing how common new primary tumours are will help us determine whether or not a tumour biomarker can be used to predict the chance of a tumour in the same breast, because such a biomarker might not be effective in predicting new, unrelated tumours," she says. In this study, Dr Kader and colleagues assembled 67 pairs of matched primary DCIS and recurrence cases to explore their genetic changes, with the goal of understanding how often a recurrence is a new tumour. The study also included a set of 32 nonrecurrent DCIS cases. The researchers performed DNA sequencing on each pair to obtain information on mutations and changes in gene copy number. They then used multiple statistical approaches to analyse the sequencing data and perform phylogenetic analyses of the tumour samples. This type of analysis allowed them to establish whether the primary DCIS and the recurrent tumours shared cancer-driving genetic events and were therefore derived from a common ancestor cell. "This is similar to building a family tree of the tumours based on the genetic events," Dr Kader says. "We can estimate how distantly related the primary DCIS and recurrence pairs are to each other and to a potential original ancestor cell, and we can track how the tumour pairs have evolved over time." The results revealed that while the majority of recurrent cases were clonal (derived from a common ancestor cell and sharing the same genetic events of the original tumour), 18 per cent of recurrent tumours were new primary lesions, unrelated to the original DCIS. "These findings can influence how patients are managed in the clinic," Dr Kader says. "For example, the occurrence of a new primary lesion in the same patient suggests a high-risk breast environment in which new tumours may develop over the years. Therefore, such patients would be candidates for preventative breast removal surgery even if the tumour is small, and they might be referred to genetic testing to ascertain whether they have any genetic predisposition." The researchers also found that four chromosomal changes and mutation in the TP53 gene were detected frequently in the recurrences related to the primary lesion, but these gene variations were not common in primary DCIS cases that don't recur and those that had non-clonal (independent) recurrence. "This particular finding from the 18 per cent of patients in our cohort who developed new, independent primary tumours raised the question of whether using these genetic biomarkers for prediction of recurrence is a good idea," Dr Kader says. "The fact that these patients did not have one of the genetic events that are more common in recurring DCIS would suggest that their risk was low, leading to undertreatment." Overall, Dr Kader says, the findings from this study suggest that when patients have an apparent recurrence from DCIS, the treatment decision should involve determining whether the recurrent lesion is related to the original tumour, as women who develop a second independent DCIS or cancer are more likely to have a higher risk of developing tumours again. "Further research is needed to understand the biology of DCIS recurrence, the progression from DCIS to invasive disease, and the role played by the tumour microenvironment and the immune system," Dr Kader says. The study was supported by the National Breast Cancer Foundation, the Cancer Council Victoria, and the Victorian Cancer Agency. Contacts: For more information contact the Peter Mac Communications team on 0417 123 048. About Peter Mac Peter MacCallum Cancer Centre is a world-leading cancer research, education and treatment centre and Australia's only public health service solely dedicated to caring for people affected by cancer.